Introduction
Voriconazole is one of the first-line therapies for invasive pulmonary aspergillosis. Many factors, such as drug-drug interactions (DDIs), erratic absorption, and continuous renal replacement therapy (CRRT), influence voriconazole exposure, resulting in high intra and interpatient variability, which is even more pronounced in critically ill patients. Voriconazole exposure is thought to be affected by extracorporeal membrane oxygenation therapy (ECMO).
However, given voriconazole’s relative lipophilicity, this understanding is based on just three ex vivo investigations and six case reports in which it was hypothesised that voriconazole sequestrates to the extracorporeal circuit. According to previously published findings, therapeutic plasma concentrations of voriconazole during ECMO cannot be assured, and the impact of ECMO on plasma levels is unknown. The goal of this study is to analyse the effect of ECMO on voriconazole systemic exposure in a large multicenter investigation to determine the necessity for dose modifications based on ECMO duration.
Methods
Critically ill patients from eight centers in four countries treated with voriconazole during ECMO support were included in this retrospective study. All adult patients hospitalized in the ICU, who were treated with voriconazole and simultaneously received ECMO-support during at least a part of this antifungal treatment, were eligible for inclusion in the study.
Patients could only be included when at least one voriconazole trough concentration was available during ECMO-support. Voriconazole concentrations were collected in a period on ECMO and before/after ECMO treatment. Multivariate analyses were performed to evaluate the effect of ECMO on voriconazole exposure and to assess the impact of possible saturation of the circuit’s binding sites over time.
Results
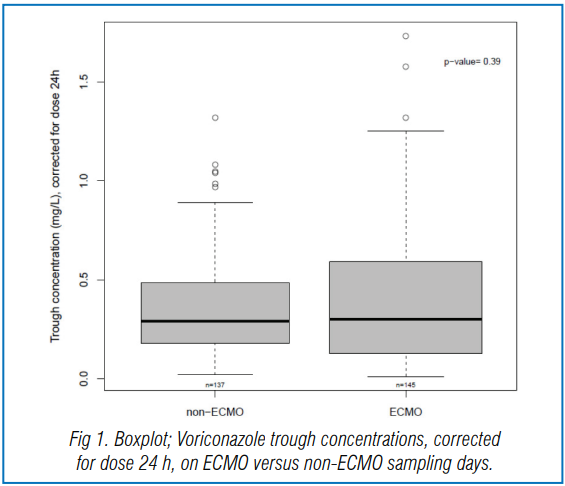
Sixty-nine patients and 337 samples (190 during and 147 before/after ECMO) were analyzed. Subtherapeutic concentrations (<2 mg/L) were observed in 56% of the samples during ECMO and 39% without ECMO (p = 0.80). The median trough concentration, for a similar daily dose, was 2.4 (1.2–4.7) mg/L under ECMO and 2.5 (1.4–3.9) mg/L without ECMO (p = 0.58).
Voriconazole trough concentrations (corrected for the administered dose 24 h previously to sampling) on ECMO and non-ECMO sampling days are depicted in Figure 1.
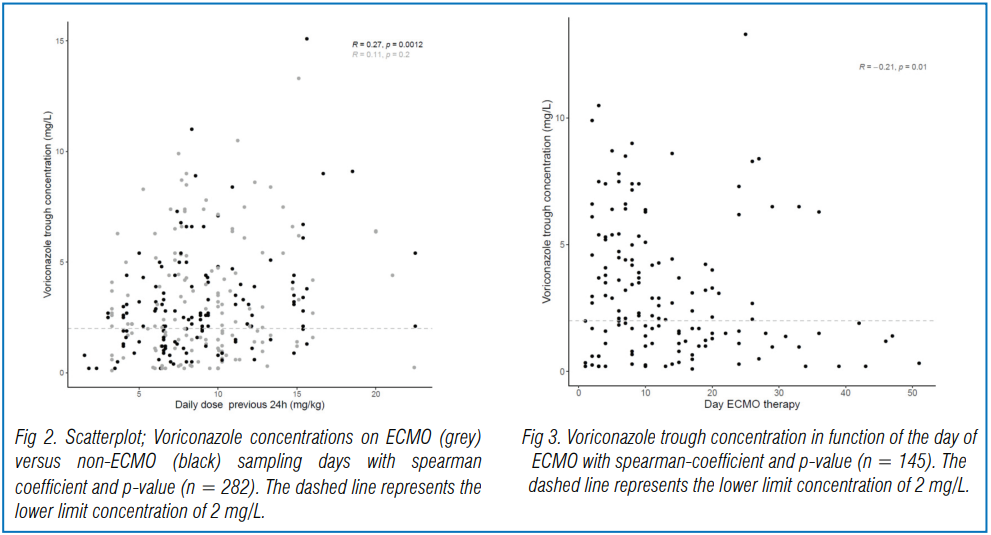
In Figure 2 and Figure 3, trough concentrations are shown in function of the administered daily dose and the day of ECMO, respectively. Extensive inter and intrasubject variability were observed. Neither ECMO nor squared day of ECMO (saturation) were retained as significant covariates on voriconazole exposure.
Conclusions
The influence of ECMO assistance on voriconazole systemic exposure is the subject of the first big, retrospective investigation. In contrast to prior ex vivo research and case reports, this study was unable to show that ECMO has an impact on voriconazole exposure. In critically ill patients, voriconazole trough concentrations were highly variable, with a substantial proportion of subtherapeutic concentrations, however ECMO had no effect on this. Therapeutic drug monitoring (TDM) of voriconazole is still crucial, especially in this severely patient population, where subtherapeutic exposure is common.
Source: Van Daele, Ruth et al. “A Large Retrospective Assessment of Voriconazole Exposure in Patients Treated with Extracorporeal Membrane Oxygenation.” Microorganisms vol. 9,7 1543. 20 Jul. 2021, doi:10.3390/microorganisms9071543




