Background
Fungal infections are a major problem affecting over one billion people annually. Emerging pathogens and increasing resistance rates are complicating the situation, while new therapeutic options remain slow to materialize. RNA-based therapeutics are changing the way we treat both genetic and infectious diseases, building on several decades of basic research. The most notable advancement in RNA-based therapeutics came as the mRNA vaccines used to limit severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Experiments with fungal plant pathogens have revealed that RNA interference can be leveraged as a tool to limit phytopathogens from destroying crops, providing a proof-of-principle that RNA-based therapeutics can fight fungi. Barriers remain to using RNA-based therapeutics against fungal infections, namely, delivery across complicated fungal cell wall structures. Extracellular vesicles may provide one solution.
Emerging fungal pathogens and rising
resistance rates necessitate new therapeutic
approaches
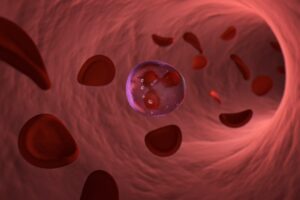
In humans, Cryptococcus gattii has proven to be a dangerous, infectious pathogen of immunocompetent individuals with poorly defined risk factors, Aspergillus fumigatus remains an ever-present danger to the immunocompromised, and Candida auris is threatening patients in hospitals with exceedingly high rates of antifungal resistance (Figure 1).

More generally, invasive fungal infections caused by the genera Aspergillus, Candida, Pneumocystis, and Cryptococcus are estimated to kill upwards of 1.5 million people per year. In the clinic, the rise of antifungal resistance is further complicating treatment of these difficult infections. The limited scope of available antifungals necessitates the development of an expanded repertoire of new drugs. One strategy that has received only cursory attention thus far is the use of RNA-based therapeutics to target human fungal pathogens.
RNA-based therapeutics are proving
useful against both genetic disorders
and infectious diseases
The variety of RNA species belonging to this group offers options that not only influence the activity of a target protein but can also modulate the genetic information, transcription, and even translation of the target gene (Figure 2).

The current roadblocks to fighting human
fungal pathogens with RNA
Several key barriers exist to the development of RNA-based therapeutics against human fungal pathogens.
(1) We need to improve our understanding of RNA regulation in human fungal pathogens to facilitate identification and exploitation of potential targets.
(2) RNA must be directed to the appropriate site of infection and limit activation of host inflammatory cascades.
(3) The RNA therapeutic must be resistant to degradation by host- or pathogen-produced RNases and be capable of entry into the fungal cell across what is oftentimes a robust cell wall.
Ultimately, specific targets within the fungal pathogen must be targeted to limit off-target effects and promote growth arrest or death of the target pathogen. Despite these challenges, numerous solutions are available that make RNA-based therapeutics a promising way forward in treating human fungal infections (Figure 3).

The way forward in fighting human fungal
pathogens with RNA
Despite the challenges, RNA-based therapeutics do offer unique advantages for the treatment of fungal infections. In particular, RNA is easy to synthesize, fast to adapt to evolving pathogens or after development of antifungal resistance, and it can offer specificity against targets at the sequence level, where variation can exist even in highly conserved pathways. Although barriers are in place, numerous innovative biochemical and biological solutions are already in development in related systems as described earlier – solutions that might be adapted for the treatment of fungal infections. Replacement of uridine with modified N1-methyl- pseudouridine in the mRNA vaccines against SARS-CoV-2 limits recognition by host nucleic acid sensors and aberrant activation of host inflammatory cascades; the nucleic acid phosphate backbone is modifiable with 2’-O-methylation to minimize immunogenicity; and advances in RNA synthesis and in vitro transcription can limit production of unwanted immunogenic byproducts such as double-stranded RNA. Combined, these developments seem likely to change the way we treat all sorts of diseases in the future, but additional research is required to see how they can be applied to the treatment of human fungal pathogens.
Conclusion
RNA-based therapeutics are rapidly changing the way we treat disease, from siRNAs-based drugs to treat liver diseases to mRNA vaccines that provide protection against SARS-CoV-2. As these treatment options mature, opportunities will become available to extrapolate these advances to the treatment of human fungal infections. We hope that by bringing attention to the possibility of using RNA-based therapeutics to treat fungal infections, the fungal research community and clinical infrastructure will be poised to adapt and quickly advance these gains into meaningful treatment options for this often devastating, but certainly under-studied class of difficult-to-treat infections.
Source: Alexander Bruch, Abdulrahman A. Kelani, Matthew G. Blango, RNA-based therapeutics to treat human fungal infections, Trends in Microbiology, Volume 30, Issue 5, 2022, Pages 411-420, ISSN 0966-842X, https://doi.org/10.1016/j.tim.2021.09.007.