Introduction
Sepsis is a life-threatening condition, and fungal pathogens are an increasingly important cause, especially in high-risk groups. During COVID-19, fungal co-infections gained significant attention due to their high morbidity and mortality.
Candida and Aspergillus are the most common fungi seen in sepsis patients. While immunocompromised states and hematologic cancers are known risk factors, age, ICU admission, frailty, chronic illnesses (like diabetes and kidney disease) also increase vulnerability.
This study aims to understand the burden of fungal pathogens in sepsis using a large Korean multicenter database focusing on prevalence, types of fungi, risk factors, and their impact on patient outcomes.
Methods
Adults aged ≥19 years with sepsis or septic shock (based on Sepsis-3 criteria) were prospectively enrolled from 20 tertiary hospitals in South Korea between September 2019 and December 2021. Data collection was part of the Korean Sepsis Alliance registry, and regular audits ensured quality. As an observational study, informed consent was waived and IRB approval was obtained from all centers.
Eligible patients were identified from emergency departments or wards. Sepsis was defined as suspected/confirmed infection with a SOFA score increase ≥2, and septic shock as hypotension requiring vasopressors with lactate >2 mmol/L despite fluids. Patients were followed until discharge or death, and detailed clinical, microbiological, and outcome data were recorded electronically.
Fungal pathogens were identified by culture, PCR, or antigen tests (β-D-glucan or galactomannan) performed within 48 hours of sepsis onset. Cancer patients included those with hematologic or solid tumors.
Statistical analysis was performed using SPSS v25. Continuous and categorical variables were compared using appropriate statistical tests. Logistic regression identified risk factors for fungal infection, and Cox regression evaluated mortality predictors. A p-value <0.05 was considered statistically significant.
Results
Among the 11,981 patients with sepsis, we analyzed 407 (3.4%) patients in whom a fungal pathogen was identified, excluding the remaining 11,574 patients with no detected fungal pathogens (Fig. 1). Of these, 251 (61.7%) patients had no hematological malignancies or solid tumors, and 156 (38.3%) patients had hematological malignancies and/or solid tumors.
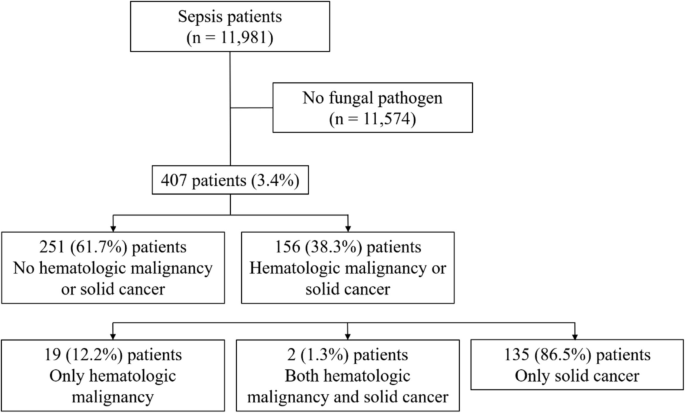
Figure 1 – Flowchart of enrolled patients.
Fungal pathogens and agents in sepsis
The most common fungi identified were Candida albicans, Candida glabrata, and Candida tropicalis. Antifungal treatment was given to 6.6% of patients, with echinocandins used more often in those with hematologic cancers.

Figure 2 – Distribution of identified fungal pathogens.
Primary infection sites and culture sources
Pulmonary infections were more common in non-hematologic cases, while abdominal and catheter-related infections were more frequent in hematologic malignancies. Culture sources differed, with sputum sampling higher in non-hematologic patients and blood, bile, and ascitic cultures higher in hematologic patients.
ICU outcomes and management
ICU admission was more common in non-hematologic patients. Other ICU treatment measures and outcomes showed no significant differences between groups.
Factors linked to fungal pathogen detection
Chronic kidney disease, connective tissue disease, immunocompromised status, and use of invasive mechanical ventilation were independently associated with fungal pathogen identification.
Factors associated with outcomes
Higher frailty, advanced age, elevated SOFA scores, and increased lactate levels were linked to higher in-hospital mortality. ICU mortality was associated with higher SOFA scores, hematologic malignancy, elevated lactate, and CRRT use.
Conclusion
Fungal pathogens were identified in 3.4% of sepsis patients, mainly among those with chronic kidney disease, immunocompromised status, and other risk factors. The low use of antifungal therapy suggests possible under-diagnosis. Improved screening, timely diagnosis, and appropriate treatment are essential, especially with rising antifungal resistance. Future work should focus on standardized diagnostics, susceptibility testing, and outcome evaluation. A coordinated, multidisciplinary approach remains key to improving survival and reducing the burden of fungal infections in sepsis.
Source: Lee, J.E., Kang, D.H., Ju, H. et al. Epidemiology and risk factors of fungal pathogens in sepsis: a prospective nationwide multicenter cohort study. BMC Infect Dis 25, 331 (2025). https://doi.org/10.1186/s12879-025-10722-y