Abstract
These recommendations for physicians who perform bronchoscopy will help to protect those patients (un)-affected by the current COVID-19 pandemic, minimize the risk of transmission, and maintain clinical care for all patients.
Considerations before Bronchoscopy
Bronchoscopy remains an important diagnostic and therapeutic tool in critically ill patients. Strict indication for performing bronchoscopies; elective procedures should be postponed. Ask about the epidemiological history, especially the history of travel and COVID-19 patient contact. Measure the temperature of the patient before the procedure (with a noncontact device if available). Nasopharyngeal swab test for SARS-CoV-2 reverse transcriptase ribonucleic acid (RT-DNA PCR) before the procedure. The patient should be categorized according to their COVID-19 status as (1) Confirmed, (2) Probable, (3) Not Probable, or (4) Negative. Patients with clinical findings for COVID-19 should be categorized as “Probable” irrespective of the result of the nasopharyngeal swab and only patients with negative nasopharyngeal swab and which is atypical for COVID-19 should be labeled as “Negative.”
Bronchoscopy in COVID-19 Confirmed or Probable Positive Patients
The indication for bronchoscopy in the case of confirmed or suspected COVID-19 disease should be made very strict and should only be considered if:
Diagnostic reason:
The nasopharyngeal smear is negative two times and clinically there is still diagnostic uncertainty of COVID-19 infection. Other diagnoses are considered that would significantly change clinical management.
Therapeutic reason:
An urgent life-saving intervention is necessary (hemoptysis, higher-grade benign or malignant central airway stenosis or foreign body aspiration). If bronchoscopy is performed for diagnostic reason, tracheobronchial lavage using a few milliliters or bronchoalveolar lavage (BAL) only is recommended. Perform procedures in natural ventilated room with air flow of at least 160 L/s per patient or ideally in negative pressure rooms with at least 12 air changes per hour and controlled direction of air flow when using mechanical ventilation. FFP3 mask (if not available FFP2 masks) should be used. The respirator should be discarded after the procedure.
Bronchoscopy in the ICU
Ventilator-associated pneumonia occurs in up to 30% patients, and accurate sampling can reduce unnecessary antibiotics.
• The cause of lobar collapse in the critical care setting is often multifactorial.
• A combination of predisposing disease-related risks, procedural impact on the lung, nonphysiological impacts of sedation, position, inadequate airway clearance mechanisms, and lack of spontaneous ventilatory effort all contribute to lobar collapse.
• High inspiratory oxygen fraction (FiO2) can in itself lead to reabsorption atelectasis through nitrogen washout.
• Bronchoscopy is commonly used in lobar and complete lung collapse during mechanical ventilation, where physiotherapy, prone positioning, or recruitment maneuvers have been unsuccessful.
• Directed suction is usually combined with forced saline flushing. If time and patient tolerance allow, exploration of the left and right bronchial tree repeatedly is advisable.
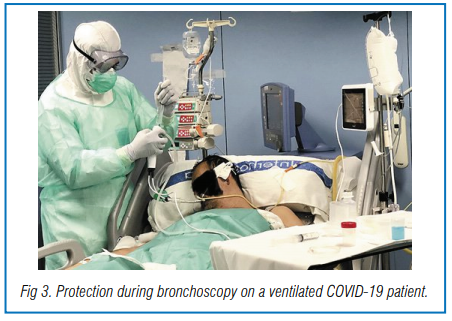
• General anesthesia with muscle relaxant is recommended in COVID-19 patients to reduce aerosol production.
• Wear disposable working cap, medical comprehensive respirator, medical mask (FFP3 or FFP2), disposable protective suit, gloves, and shoe cover.
• Emergency drills including cardiac resuscitation protocols for the COVID-19 patient should be noted for safe adoption in need.
• For patients with intubation and mechanical ventilation, FiO2 should be adjusted to 100%. Volume control, pressure-limited mode, is preferred and PEEP should be kept at the same level during the procedure.
Case Study
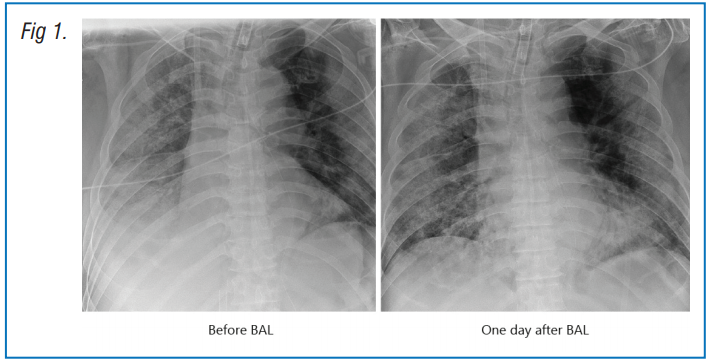
Male patient, aged 66 years was admitted to hospital presenting with cough and fever for 10 days. He had COPD and hypertension. The patient was intubated and ventilated following progressive hypoxemic respiratory failure despite high-flow nasal oxygen therapy (HFNO). Veno-venous ECMO was instituted on day 2 due to refractory severe acute respiratory distress syndrome (SARDS). Chest radiography demonstrated worsening opacification in the right low zone. Hence, bronchoscopy was performed on day 4. Therapeutic BAL was performed in the right lower lobe basal segments. A large quantity of mucus was cleared. A chest X-ray the following day showed clearing of the lung fields and restored visibility of the right hemidiaphragm. (Fig 1)
• Monitor the SpO2 during the procedure and stop the procedure if SpO2 drops. Avoid BAL in patients with obvious hypoxia (SpO2 <92%, especially if already on supplemental oxygen support).
• For the patient on veno-venous ECMO support, anticoagulation should have been stopped a few hours before the procedure, and clotting time tested pre-procedure.
• Platelets should be >50/µL. BAL may be performed. Therapeutic lavage will help to wash out the mucus in the distal airway (Fig. 3).
Specimens should be stored and processed according to the biosafety requirement. A negative pressure suite with at least 10 cycles/h exchange is preferred for the procedure if possible. Otherwise, the examination room should be disinfected and an air disinfection machine may be applied. All staff must remove personal protective equipment according to the appropriate training and leave the examination area only after ensuring strict hand hygiene.
Postprocedural Necessities
Following completion of the bronchoscopy, a review of the patient and physiological parameters as well as the ventilator settings (particularly delivered volume) is advised. A short recruitment maneuver may be necessary to improve oxygenation, and a chest radiograph should be ordered to exclude a pneumothorax. Where possible utilize disposable single-use bronchoscopes if timely and validated reprocessing of the bronchoscopes is not ensured. If timely and validated reprocessing of the bronchoscopes is ensured, the reprocessing process for disinfecting the devices does not have to be changed. However, the bronchoscope should be transported and sterilized separately from other patients.
Source: Luo F, Darwiche K, Singh S, Torrego A, Steinfort D, P, Gasparini S, Liu D, Zhang W, Fernandez-Bussy S, Herth F, J, F, Shah P, L: Performing Bronchoscopy in Times of the COVID-19 Pandemic: Practice Statement from an International Expert Panel. Respiration 2020;99:417-422. doi: 10.1159/000507898




